American researchers presented long-term results from a clinical trial of a minimally invasive transcatheter deep vein arterialization system for the lower leg in patients with severe leg ischemia and non-healing ulcers who were at risk of amputation and were unable to undergo conventional revascularization. During this trial, some participants died from various causes; among the survivors, 68 percent avoided amputation. A paper describing the study's findings was published in The New England Journal of Medicine.
Peripheral arterial disease is a critical narrowing of the vessels supplying peripheral organs and tissues. The primary mechanism of narrowing is atherosclerosis, but inflammation (endarteritis), thrombosis, and vasospasm can also contribute. In the vast majority of cases, the legs are affected, with intermittent claudication during walking a characteristic symptom; in severe ischemia, pain is present even at rest. The most severe form of the disease—critical lower extremity ischemia (CLEI, stages 5–6 according to the Rutherford classification)—is characterized by pain at rest, non-healing trophic ulcers, or gangrene. The treatment of choice is intravascular (stent) or surgical revascularization, but approximately 20 percent of patients are unable to undergo this procedure due to vascular anatomical features or the extent of the lesion. These patients often require high limb amputation.
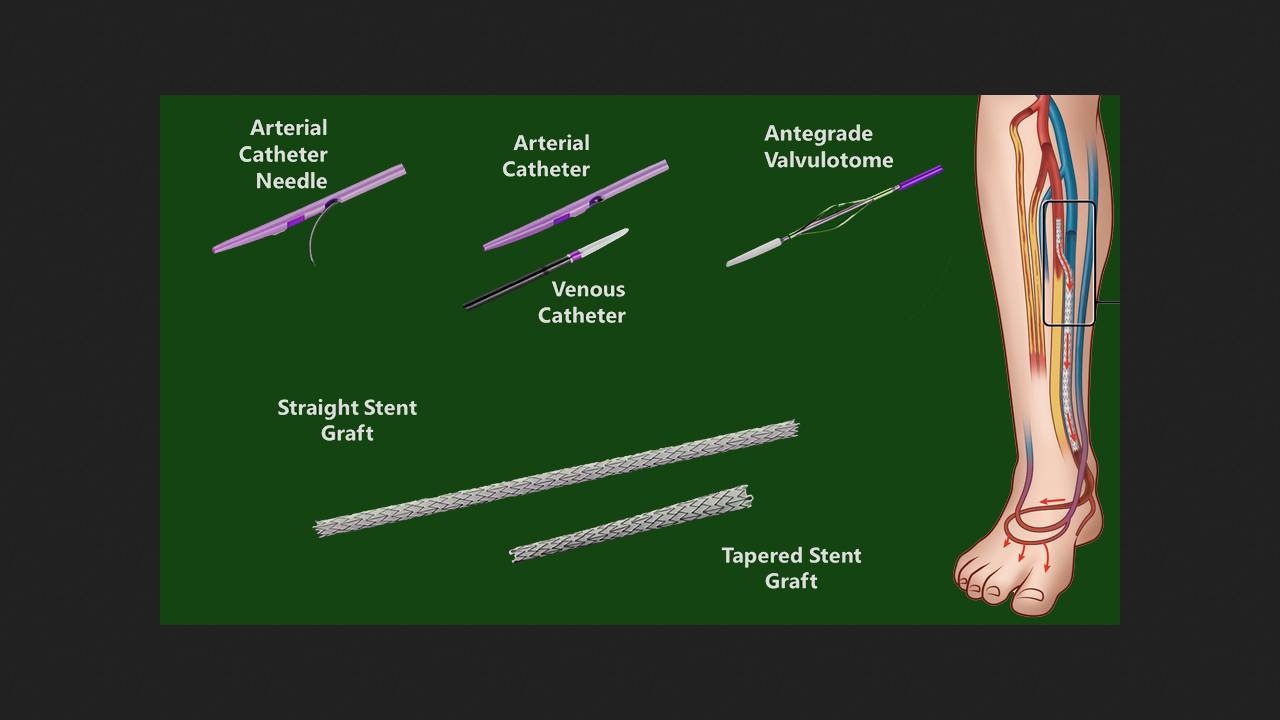
Since 1912, deep vein arterialization (DVA) has been a treatment for CLI. This involves redirecting oxygenated arterial blood into the venous circulation of the lower leg and foot. Performing this through an open surgical approach carries a clinically unacceptable risk of complications, and various off-label systems for percutaneous endovascular interventions have been used for this purpose with varying success. The LimFlow system was developed specifically for the minimally invasive treatment of CLI in patients with no other options and a risk of amputation. It includes arterial and venous catheters for ultrasound-guided vascular anatomy and ensuring mutual access between them, an antegrade valvulotome for venous valve removal, and self-expanding stent prostheses for diverting arterial blood into the veins. Early trials of the system have yielded encouraging results.
Mehdi Shishehbor, director of the Harrington Cardiovascular Institute at University Hospitals Cleveland, along with colleagues and Stryker Inari Medical, presented the results of a two-year follow-up of participants in the multicenter, prospective, open-label, non-randomized pilot trials PROMISE I and PROMISE II. During these trials, 137 patients (mean age 69 years; 68 percent men) with CLI, non-healing ulcers or gangrene, and no other treatment options underwent deep vein arterialization using LimFlow. Ninety-one percent of the participants had hypertension, and 75 percent each had diabetes and dyslipidemia.
By the second year of the intervention, 28 participants had died from various causes (including five from COVID-19 and four from chronic kidney disease), and 38 had undergone amputation of the affected limb. Overall survival was 72 percent, amputation-free survival was 49 percent, and limb salvage was 68 percent. Of the 49 patients who retained limbs at this time, 38 showed improvement according to the Rutherford classification, including 26 who achieved stage 0 (no ischemia). In 82 percent of patients, chronic wounds were independently assessed as healed (71 percent) or healing (12 percent). Pain scores on a 0-10 digital analog scale decreased from a median baseline of 6 to 0 (a median reduction of 4.3 points).
Thus, deep vein arterialization with LimFlow provides a lasting effect, allowing limb preservation, healing of skin defects, and pain relief in most patients. The system has already been approved for use.
Previously, British scientists conducted a population-based study and found that the risk of major amputation after revascularization of leg arteries is increased in younger patients with complicated disease, diabetes, other comorbidities, or after unplanned surgery distal to revascularization.