Neuroscientists have described a mechanism involved in the development of treatment-resistant depression. In experiments on marmosets, they showed that inhibiting the dorsolateral prefrontal cortex (dlPFC) leads to decreased motivation and increased anxiety, but the effect depends only on the left hemisphere. They then demonstrated how the dlPFC is connected to two regions of the subcallosal cingulate cortex and reversed the effect by administering ketamine to one of these regions. The study was published in Science.
Transcranial magnetic stimulation of the dorsolateral prefrontal cortex (dlPFC), whose activity is reduced in the disorder, is used to treat treatment-resistant depression. This stimulation reduces symptoms of depression and anxiety and normalizes the characteristic hyperactivity of neurons in area 25 of the subcallosal cingulate cortex (scACC). Stimulation of the dlPFC region associated with Brodmann area 46 is most effective: activity in this area negatively correlates with activity in area 25. However, the mechanisms by which the dlPFC and scACC interact remain unclear.
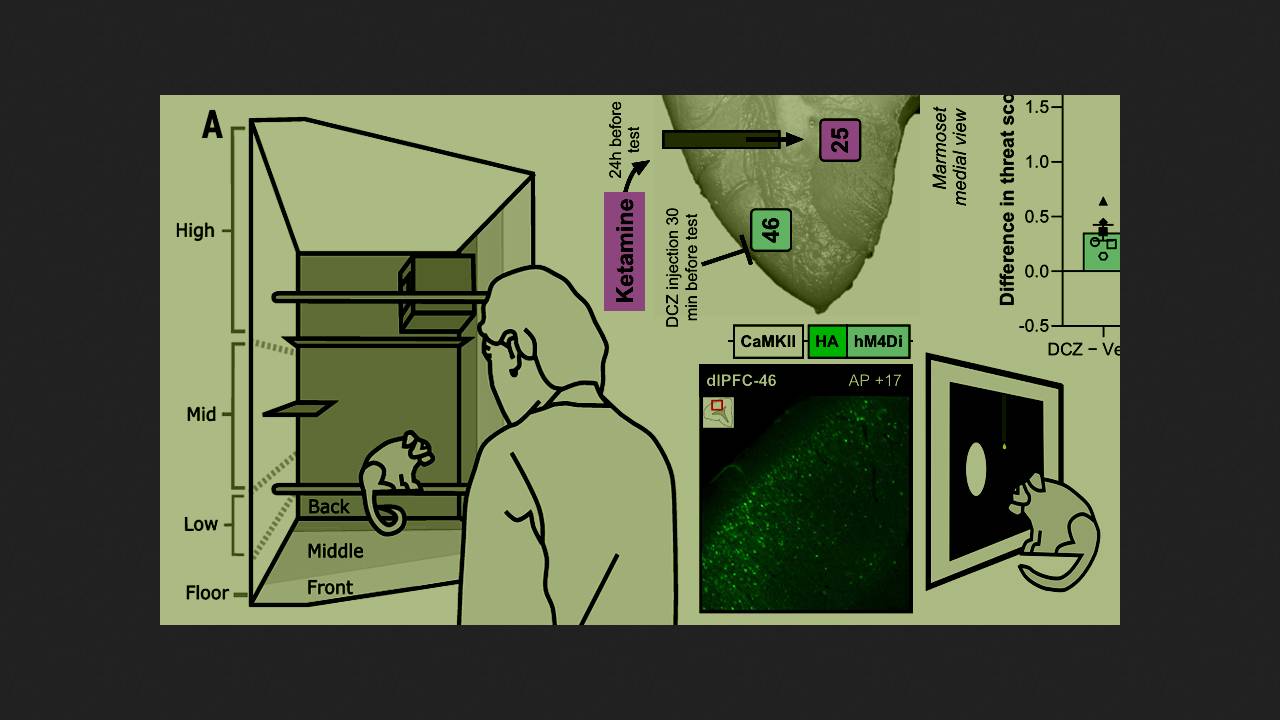
To understand this, a team of scientists from the University of Cambridge, led by Christian M. Wood, conducted experiments with common marmosets (Callithrix jacchus). First, they assessed the motivation of six monkeys to press a button on a touchscreen to receive a milkshake as a reward. After each reward, the marmosets were required to press the button more times than before to receive the next milkshake. The scientists then chemogenetically inactivated neurons in area 46. After this, the marmosets' motivation decreased: they stopped pressing the button earlier and, consequently, received fewer milkshakes. Pressing speed and appetite did not change—the primates simply gave up faster.
Since a similar blunting of motivation had previously been observed with hyperactivity in area 25, the researchers injected ketamine, a drug used for anesthesia and sometimes to treat resistant depression, into the area. It blocked the decrease in motivation caused by the suppression of area 46 neurons. Areas 25 and 46 are connected by another region of the cingulate cortex, area 32: its neurons receive signals from area 46 and project to area 25. Chemogenetic inactivation of area 32 neurons also reduced motivation in marmosets, but ketamine injected into area 25 reversed this effect. If the marmosets' neurons were not inhibited, ketamine administration did not change their behavior.
The scientists then tested the relationship between the three fields and anxiety, which often accompanies depression, and transcranial stimulation of the dlPFC typically reduces it. Hyperactivity in field 25 is known to increase the sensitivity of marmosets to threats. To induce anxiety, a stranger stood next to the cage for two minutes. In response, the animals froze and vocalized anxiously. Chemogenetic inactivation of field 46 or 32 increased the anxiety response.
The scientists then tested for functional asymmetry and found that motivation and anxiety were affected by dysfunction of the dlPFC and scACC in the left hemisphere alone. When the scientists inactivated area 46 on the left side only or on both sides, the marmosets became more anxious, but inactivation of the right area 46 had no effect on the monkeys' behavior. The same was true for motivation, but in this case, the scientists targeted the left area 32. This is consistent with the fact that left-sided transcranial stimulation of the dlPFC is more commonly used in the treatment of depression, presumably due to its greater effectiveness.
Thus, a functional network that regulates motivation and anxiety operates in the left hemisphere of marmosets. It includes the dorsolateral prefrontal cortex, related to area 46, and areas 25 and 32 in the subcallosal cingulate cortex. These findings help us understand how symptoms of treatment-resistant depression develop and how transcranial stimulation and ketamine can alleviate them.
Previously, scientists showed that a drug used for Parkinson's disease can help with treatment-resistant depression, but only in combination with antidepressants.