Chinese researchers reported success in a phase II clinical trial of anti-CLDN18.2 chimeric antigen receptor T cells in refractory gastric and gastroesophageal junction cancer. The therapy significantly extended patients' lives, according to a trial report published in The Lancet.
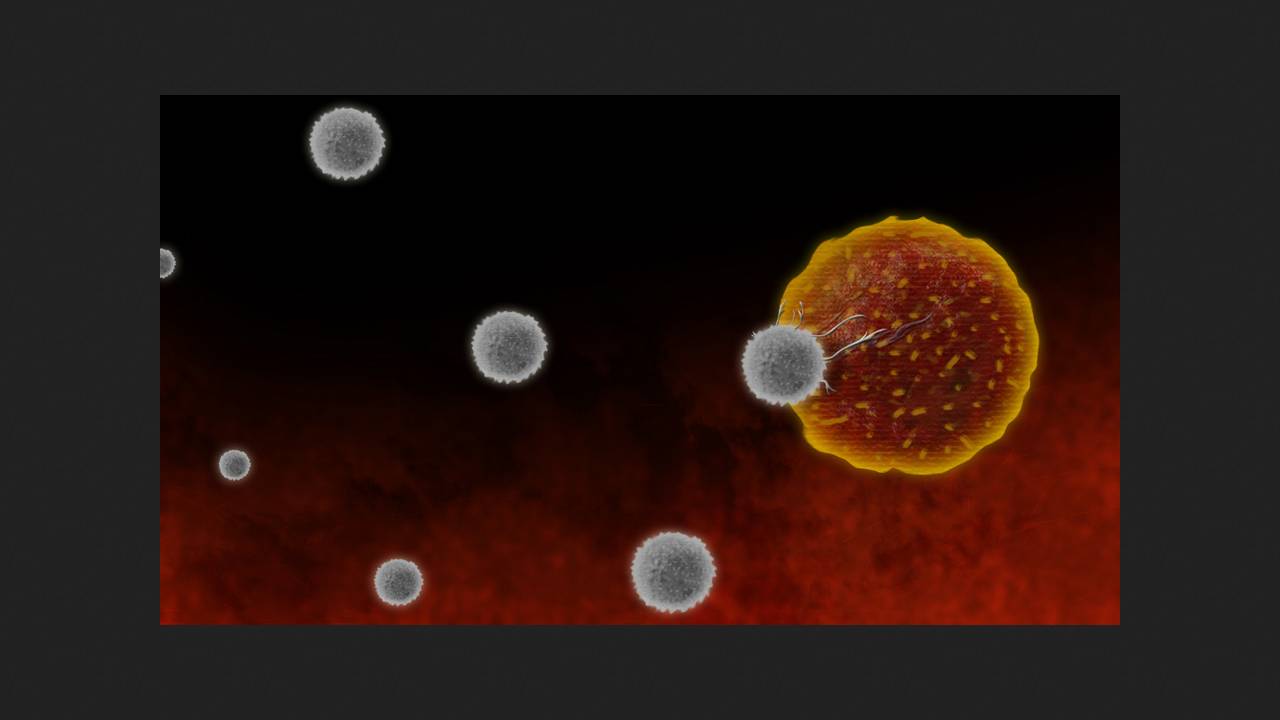
Chimeric antigen receptor T-cell technology (we discussed CAR-T cells in detail in the article "Chimera vs. Cancer") can achieve long-term remission and even complete cures in many patients who have failed other therapies. Due to certain limitations of its first generations, only six drugs have reached clinical use for the treatment of B-cell hematologic malignancies and one for the treatment of a solid tumor—a type of synovial sarcoma. CAR-T therapy for other tumors is currently in various stages of preclinical and clinical trials.
Gastric and gastroesophageal junction cancer is the fifth most common cancer in terms of incidence and mortality. Approximately 40 percent of patients with these tumors strongly express claudin-18 isoform 2 (CLDN18.2). This is a protein found in tight junctions of epithelial cells and is specific to the gastric epithelium. Due to their location, tight junctions in healthy epithelium are inaccessible to the action of biologic drugs, but CLDN18.2 in tumors can serve as a therapeutic target. Zolbetuximab, a monoclonal antibody to this protein, is already used for CLDN18.2-positive gastric cancer in addition to chemotherapy; it requires regular administration. The autologous CAR T-lymphocyte drug satricabtagene autoleucel (satri-cel, CT041) also targets this target and has demonstrated satisfactory tolerability and potential efficacy in phase I trials.
Changsong Qi of Peking University, along with colleagues and collaborators from CARsgen Therapeutics, conducted the open-label, randomized phase II trial T041-ST-01 at 24 Chinese clinical centers. They enrolled 156 adult patients with HER2-negative, CLDN18.2-positive, refractory, unresectable gastric or gastroesophageal junction adenocarcinoma. Following lymphodepletion, 104 of them received up to three infusions of satri-cel at a dose of 250 million cells; the remaining 52 received standard therapy with nivolumab, paclitaxel, docetaxel, irinotecan, or rivoceranib, at the physician's discretion.
In the main group, 27 percent of participants had previously received three or more cycles of chemotherapy, and 69 percent had peritoneal metastases. In the control group, these figures were 19 and 60 percent. The median overall survival with satri-cel was 7.92 months versus 5.49 months with standard treatment (p = 0.0416), and the progression-free survival was 3.25 versus 1.77 months (p < 0.0001). Serious adverse events were reported in 99 percent of participants in the main group (most commonly, a decrease in the level of total leukocytes, lymphocytes, or neutrophils) and 63 percent in the control group. Cytokine release syndrome developed in 95 percent of patients after satri-cel administration. The obtained results allow us to consider the use of satri-cel as a third-line therapy for advanced refractory HER2-negative, CLDN18.2-positive gastric and gastroesophageal junction cancer. Its use in earlier stages of similar tumors merits further study, the authors conclude. Previously, American researchers presented the results of a pilot trial of next-generation CAR-T lymphocytes in recurrent glioblastoma, which involved three patients. The tumors rapidly shrank in all participants, but subsequently recurred in two.