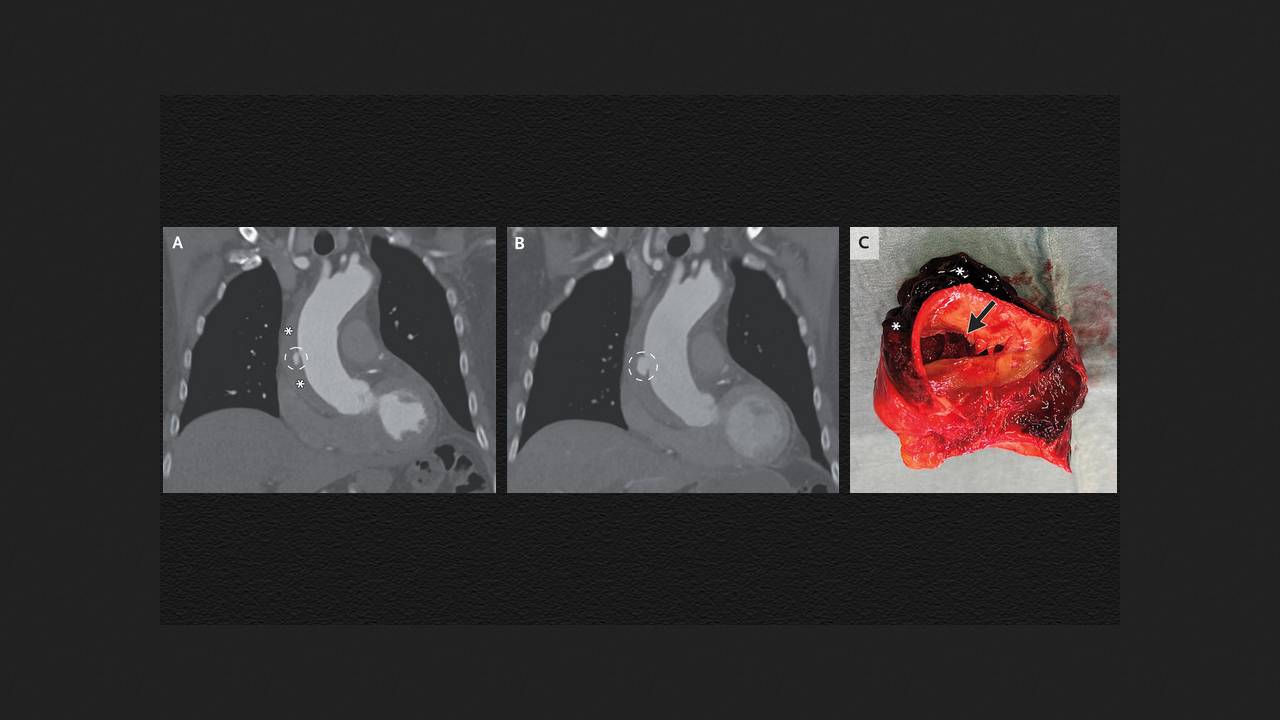
An 80-year-old man with an unremarkable medical history was admitted to the emergency department of a Dutch hospital with complaints of chest pain for 12 hours and elevated D-dimer levels (a marker of recent thrombosis). His blood pressure was 147/92 mmHg, his pulse was 70 beats per minute, and his physical examination was normal. A pulmonary computed tomography angiography (CT angiography) did not reveal pulmonary embolism, but it did show an ulcer-like lesion on the ascending aorta and an intramural hematoma extending to the arch and upper portion of the descending aorta. Drs. Sjoerd Bouwmeester and Andrew Tjon Joek Tjien of the Katharina Hospital in Eindhoven shared this case in The New England Journal of Medicine.
The man was diagnosed with an intramural aortic hematoma, a form of acute aortic syndrome in which blood enters the medial tunica of the vessel, forming a thrombus that bulges the vascular wall outward. This condition is associated with an increased risk of aortic dissection. The patient was started on intramural fluid therapy to reduce blood pressure and heart rate. His chest pain resolved, and he was transferred to the cardiac center. After discussing the matter with the patient, the doctors decided against immediate surgery and continued observation. A CT scan three days later revealed an enlarged ulcer-like lesion, and the man underwent open surgery to replace the ascending aorta over the coronary vessels and half of the aortic arch. In addition to the hematoma, the excised portion of the vessel revealed a rupture of the medial tunica and a dissection of the ascending aorta. The patient was discharged from the hospital six days after the surgery.