An international scientific team reported the success of a phase III clinical trial of depemokimab for chronic rhinosinusitis with nasal polyps. This monoclonal antibody to interleukin-5 is administered semiannually. A report on the study was published in The Lancet, where an editorial was also dedicated.
Long-term inflammation associated with chronic rhinosinusitis with nasal polyps (CRNSP) leads to damage and abnormal regeneration of the mucous membranes of the nose and sinuses. This results in persistent or recurring symptoms such as nasal congestion, runny nose, facial pain or pressure, and loss of smell, as well as polyp growth. This condition is typically treated with topical glucocorticoids, sometimes combined with surgical removal of the polyps. However, long-term use of such medications is associated with an increased risk of side effects and is not always effective, and polyps often regrow after removal.
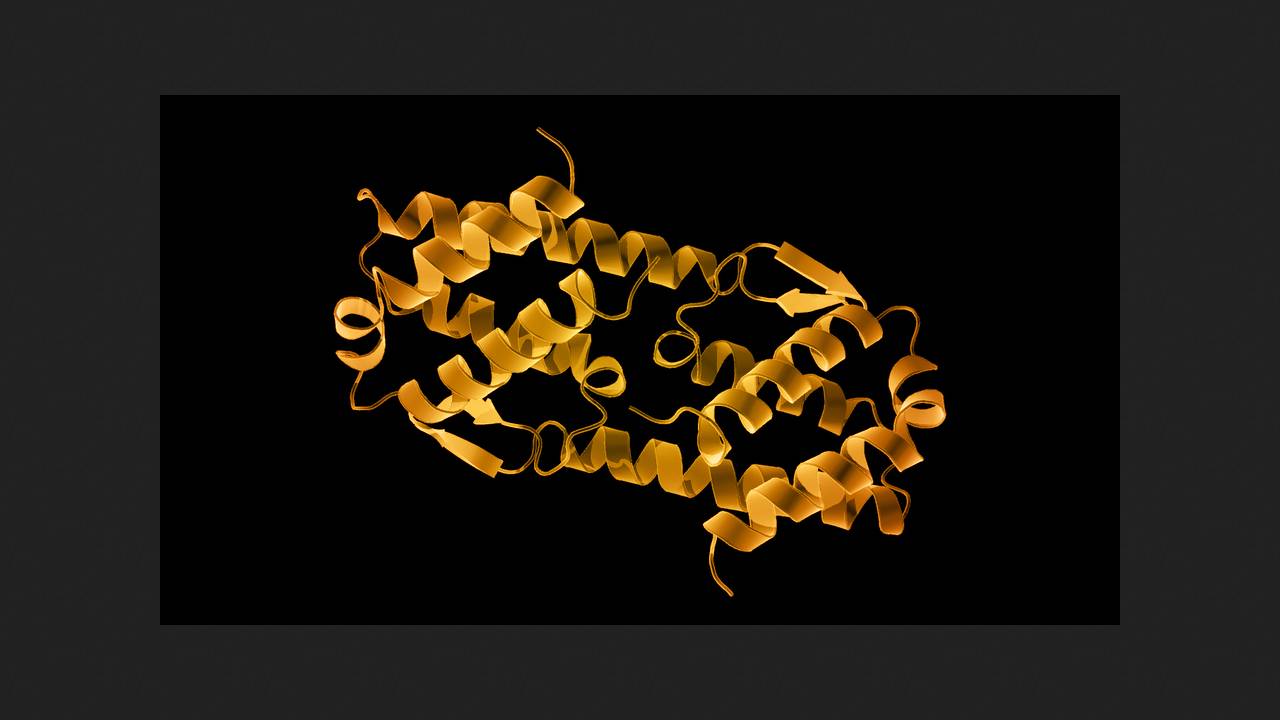
The most common cause of CRSNP (up to 85 percent of cases) is type 2 inflammation. Its mediators are certain cytokines, such as interleukins 4, 5, and 13. With this in mind, biologic drugs (monoclonal antibodies) that target inflammatory mechanisms have been developed and introduced as adjuvant therapy for severe forms of the disease. These drugs include dupilumab (binds the alpha subunit of the interleukin 4 receptor and was recently approved for use in chronic obstructive pulmonary disease), mepolizumab (binds interleukin 5), and omalizumab (binds immunoglobulin E). All are administered every 2–4 weeks. Depemokimab (GSK3511294) has become the first ultra-long-acting anti-interleukin 5 drug, with pharmacokinetics that ensure an effect lasting six months after injection. It has previously demonstrated efficacy in severe bronchial asthma in clinical trials.
Philippe Gevaert of Ghent University and colleagues, sponsored by GlaxoSmithKline, conducted the double-blind, randomized, placebo-controlled phase III trials ANCHOR-1 and ANCHOR-2 at 190 clinical centers in 16 countries. A total of 528 adult patients with decompensated CRSNS, bilateral polyps with an endoscopic score of at least five out of eight, severe clinical manifestations, and a history of either systemic glucocorticoid therapy, surgery, or both.
Two hundred seventy-two participants were randomly administered 100 milligrams of depemokimab subcutaneously twice, 26 weeks apart, while the remaining 256 received placebo. Follow-up continued for 52 weeks from the first injection. All participants also received standard glucocorticoid therapy, administered intranasally and, if needed, short courses of systemic glucocorticoids, as well as saline nasal irrigation. At the beginning and end of the study, subjective assessments were made, symptom severity was assessed, endoscopy and CT scans were performed, and blood samples were collected for analysis of the drug's pharmacodynamics and immunogenicity.
By week 52 of observation, depemokimab administration in both trials resulted in significant improvements in mean endoscopic polyp and nasal obstruction scores. The incidence of adverse events did not differ statistically significantly between the intervention and control groups.
Thus, the addition of twice-yearly depemokimab injections to standard therapy improves clinically significant CRS outcomes compared with placebo and is well tolerated, supporting its use for this indicator, the authors conclude.
Previously, clinical trials of benralizumab, a monoclonal antibody to the alpha subunit of the interleukin-5 receptor, were conducted, which showed that it is superior to the glucocorticoid prednisolone in relieving exacerbations of bronchial asthma and chronic obstructive pulmonary disease accompanied by eosinophilia.