American and Australian researchers conducted randomized clinical trials and found that sodium oxybutyrate effectively reduces the symptoms of spasmodic dysphonia in patients who experience relief after drinking alcohol. The report was published in the Annals of Neurology.
Spasmodic dysphonia (laryngeal dystonia, laryngeal dystonia) is an idiopathic neurological disorder characterized by involuntary spasms of the laryngeal muscles, typically during speech. This causes the voice to become tense, intermittent, hoarse, or creaky, which can lead to communication and social difficulties, as well as psychological problems of varying severity. The condition typically develops between the ages of 30 and 50 and is slightly more common in women than in men. Treatment includes botulinum toxin injections into the lower esophageal sphincter or surgically transecting the laryngeal nerve, but these methods are not effective for everyone and often have side effects. However, some patients report a noticeable reduction in spasms after drinking small amounts of alcohol.
Sodium oxybutyrate is a salt of gamma-hydroxybutyric acid (GHB), which serves as a brain-penetrating biochemical precursor of the inhibitory neurotransmitter gamma-aminobutyric acid (GABA). It has sedative and muscle relaxant effects, with some effects at low doses similar to those of alcohol intoxication. The drug is used in different countries for different indications and in different doses: orally in relatively small doses for catalepsy and narcolepsy, as well as for alcohol withdrawal syndrome; intravenously in large doses for short-term or induction of anesthesia.
Kristina Simonyan of Harvard Medical School and colleagues conducted a double-blind, randomized, placebo-controlled, crossover phase IIb trial. They enrolled 106 patients (74 of whom were women) with laryngeal dystonia. The average age was 58.6 years, and the average disease duration was 16 years. Ninety-two participants had previously received botulinum toxin injections, and 23 had received pharmacological therapy (but not during the trial).
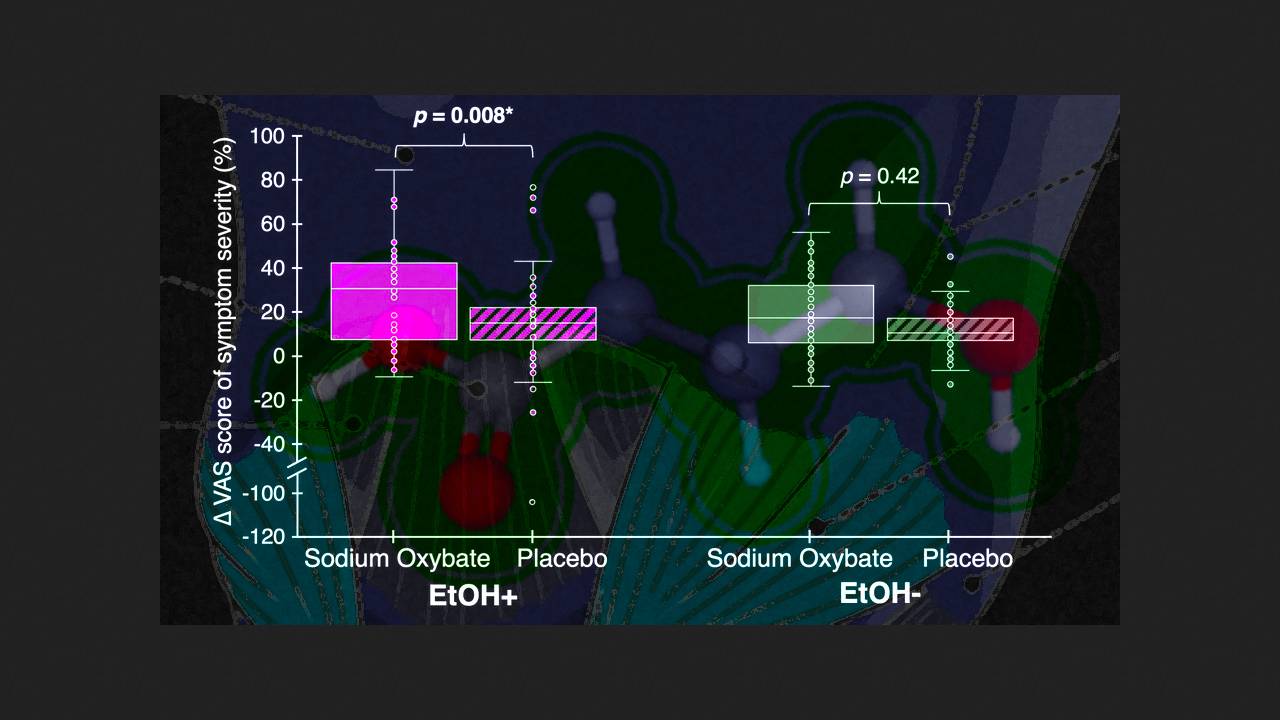
All patients underwent a standardized ethanol challenge at a dose of 0.8 grams of 40-proof vodka per calculated liter of total body water. The effect was assessed by the number of speech pauses characteristic of the disease in each sentence, voice properties, breathiness, and tremor 15–120 minutes after administration. Symptom reduction was observed in 50 participants. Following this, patients were randomly assigned to receive a single oral dose of 1.5 grams of sodium oxybutyrate or placebo, followed by the opposite the following day, and symptoms were recorded 40 minutes later. Changes from baseline were assessed using a linear mixed-effects model based on restricted maximum likelihood.
Sodium oxybutyrate was found to significantly reduce symptoms (by an average of 40.81 percent; p = 0.008) in participants with a positive alcohol response, while the effect was insignificant in those without a response (p = 0.42). The drug's effects gradually wore off over 300 minutes without rebound effects. Cognitive function, suicidal tendencies, and vital signs were unaffected; the main side effects included mild dizziness, nausea, and drowsiness.
Thus, sodium oxybutyrate may produce clinically significant improvement in a subpopulation of patients with alcohol-responsive spastic dystonia and serve as the first pathophysiologically relevant oral drug for its treatment. The authors are currently conducting phase III trials.
Previously, American scientists grew a model of vocal cords from human induced pluripotent stem cells that were capable of producing sounds and even responding to tobacco smoke.