Researchers from ten countries reported success in clinical trials of mirikizumab for moderate to severe active Crohn's disease. The study was published in The Lancet.
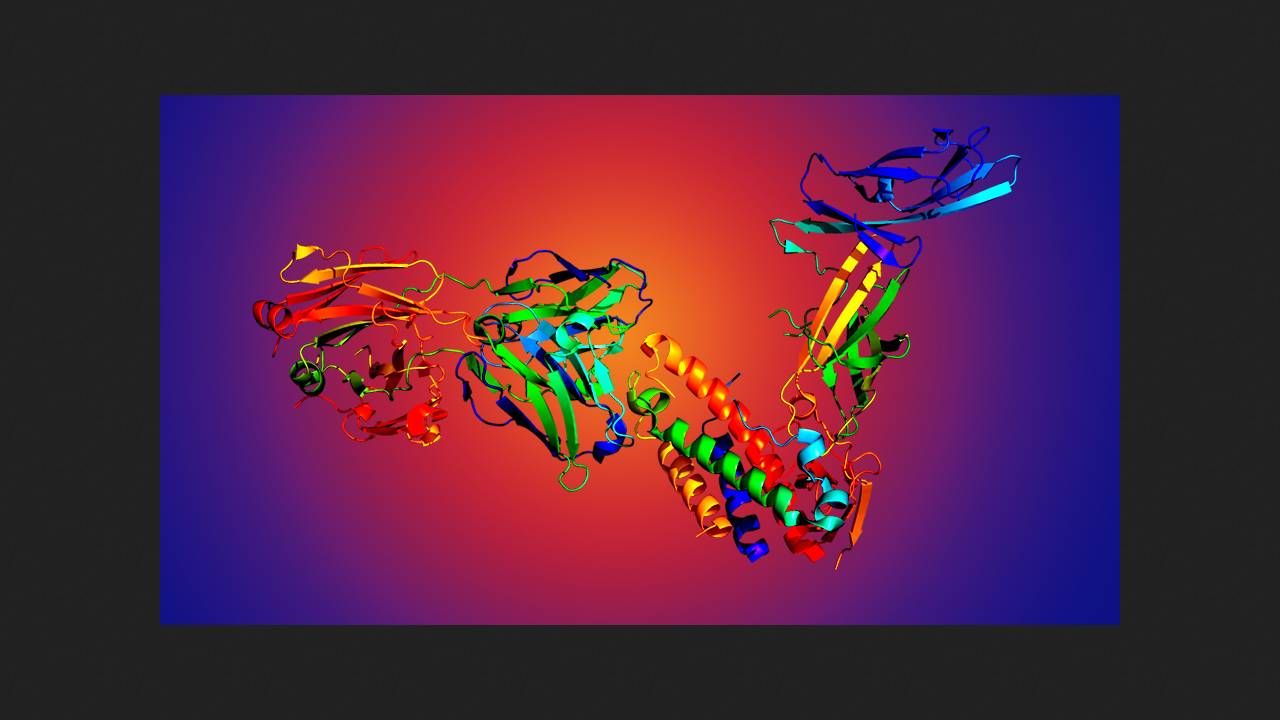
Crohn's disease is a severe chronic inflammatory disease of the gastrointestinal tract, primarily the intestines. It is caused by complex interactions between the gut microbiota and the patient's immune system. Available medications are not always effective, preventing patients from restoring their quality of life and ability to work to an acceptable level. Some patients require intestinal surgery. Mirikizumab is a monoclonal antibody to the alpha subunit of interleukin-23, which is produced by macrophages and dendritic cells. The drug is already used for another chronic inflammatory bowel disease, ulcerative colitis.
Marc Ferrante of the Catholic University of Leuven and colleagues from nine countries conducted the double-blind, randomized, controlled phase III VIVID-1 trial at 324 clinical centers in 33 countries. They enrolled 1,065 adult patients with moderate to severe Crohn's disease resistant to current therapy. They were randomly assigned in a 6:3:2 ratio to receive either mirikizumab at a dose of 900 milligrams intravenously at weeks 0, 4, and 8, then 300 milligrams subcutaneously every four weeks until week 52; ustekinumab (an approved monoclonal antibody to interleukin-12 and -23) at a dose of six milligrams per kilogram of body weight intravenously at week 0, then 90 milligrams subcutaneously every eight weeks until week 52; or placebo.
The primary endpoints of the trial were the superiority of mirikizumab over placebo, based on a combination of patient-reported subjective clinical improvement at week 12 and either endoscopic response at week 52 or clinical remission as measured by the CDAI score at the same time. Risks were calculated after adjustment for confounding factors, and comparisons were made using the Cochran-Mantel-Haenszel test.
Both primary endpoints were achieved. By week 52, endoscopic remission was observed in 38 percent of patients receiving mirikizumab and 9 percent receiving placebo (99.5 percent confidence interval for the difference, 20.6 to 36.8 percentage points; p < 0.0001). Clinical remission according to CDAI was achieved in 45.4 percent versus 19.6 percent (99.5 percent confidence interval for the difference, 15.9 to 35.6 percentage points; p < 0.0001). Efficacy was comparable with ustekinumab. The most common adverse event during therapy was COVID-19 (trials were conducted from July 2019 to August 2023). Serious adverse events developed in 10.3 percent of patients in the mirikizumab group; 10.7 percent were treated with ustekinumab and 17.1 percent with placebo. The safety profile of mirikizumab was consistent with its known adverse event profile. Based on the trial results, the drug was deemed safe and effective for the induction and maintenance treatment of patients with moderate to severe Crohn's disease who are intolerant or inadequately responsive to standard therapy. A Swedish population-based study previously showed that inflammatory bowel diseases are associated with an increased risk of developing heart failure within 20 years of diagnosis, with this risk being higher in Crohn's disease than in ulcerative colitis.