Proton therapy primarily uses pencil beam scanning (PBS) for precise dose distribution. However, this method is limited by the number of beam directions that can be delivered within a reasonable treatment time. Proton arc therapy (PAT) addresses this issue by using an arc trajectory. PAT differs from PBS in that it offers a greater number of beam angles and the ability to optimize energy for each direction, reducing treatment time.
Researchers from the Trento Proton Therapy Center, together with colleagues from RaySearch Laboratories, compared the dosimetric parameters of proton arc therapy plans with modern multi-field optimized pencil beam scanning (MFO PBS) plans. The study involved 10 patients with head and neck cancer. This location was chosen due to the large number of vital organs located near the tumor, which can be protected using the new technique.
In the future, PAT treatment is planned to be performed with the beam turned on during gantry movement (dynamic mode). This means that all system parameters will need to be automatically adjusted while the structure is rotating. Due to the complexity of the equipment and software, this treatment is not yet used in hospitals. Instead of using dynamic PAT, the scientists employed a simpler, static approach. They divided the arc into several PBS beams and used a conventional radiation delivery method. Using RayStation software, they created MFO plans (with six beam directions) and PAT plans (with 30 beam directions), optimized to minimize errors.
It turned out that the new PAT plans were much better at targeting radiation to the tumor than the older MFO methods. Although both methods covered the affected tissue equally well, PAT reduced the dose to vital organs.
This was particularly noticeable in the brainstem, where the dose decreased by 19.6 units (Gy (RBE)) at maximum and by 9.5 on average. For other nearby organs, the difference was insignificant, but PAT significantly reduced the dose for those organs located far from the tumor.
Scientists also studied how differences in radiation exposure affected the likelihood of side effects. It turned out that PAT reduced the risk of dry mouth by 8.5%, as well as slightly reduced the likelihood of other problems, such as difficulty swallowing, the need for tube feeding, and increased salivation.
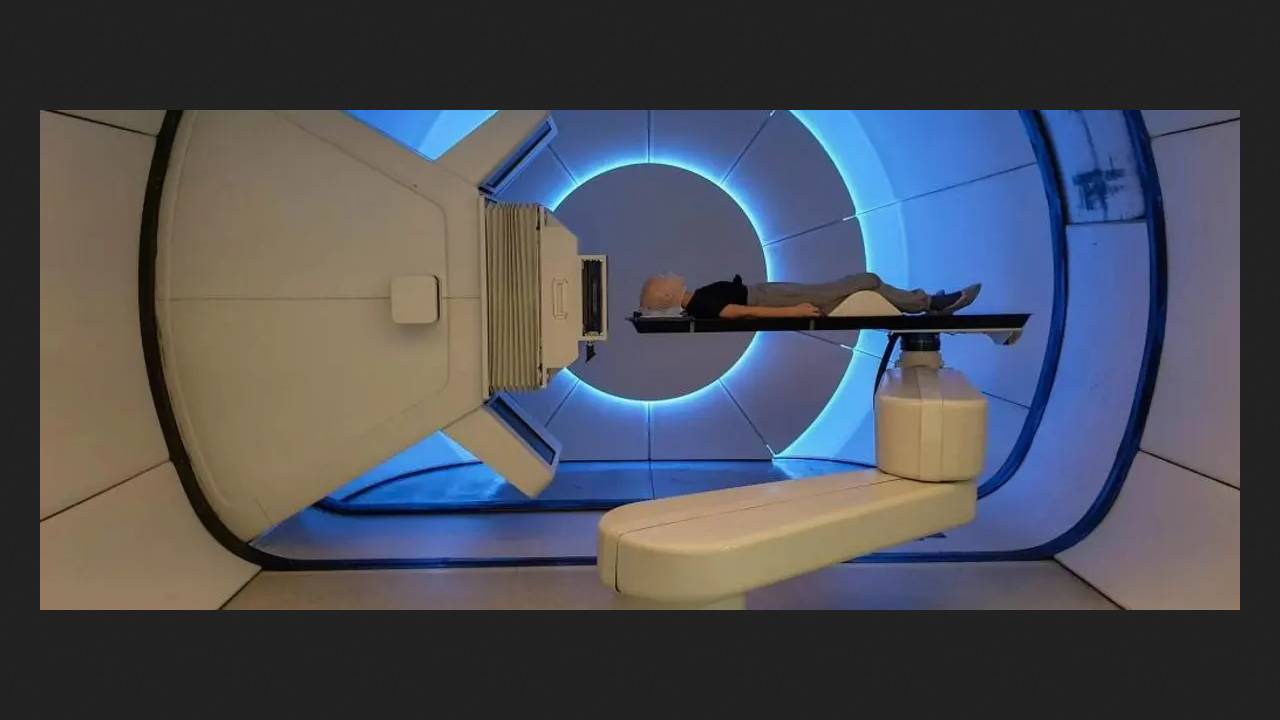
To test the feasibility of using PAT in a real-world hospital, the team irradiated one patient using both MFO and PAT plans on a clinical gantry. The irradiation time was found to be nearly identical: 36 minutes for PAT (30 directions) and 31 minutes for MFO. Reducing the number of directions to 20 reduced the time to 25 minutes, while maintaining virtually the same irradiation quality.
Nine patients have already received or are receiving PAT treatment: five with head and neck tumors, three with brain tumors, and one with breast cancer. The first two patients with head and neck tumors were assigned PAT plans with a half-arc (180°) and 10 beam directions, with a mean treatment time of 12 minutes. The next two patients received treatment with a full-arc (360°) and 20 beam directions, with a mean treatment time of 24 minutes. Quality control showed a high compliance rate (99.6%), with only one patient requiring plan adjustment. The researchers plan to determine whether this method reduces toxicity and are working to reduce delivery time.