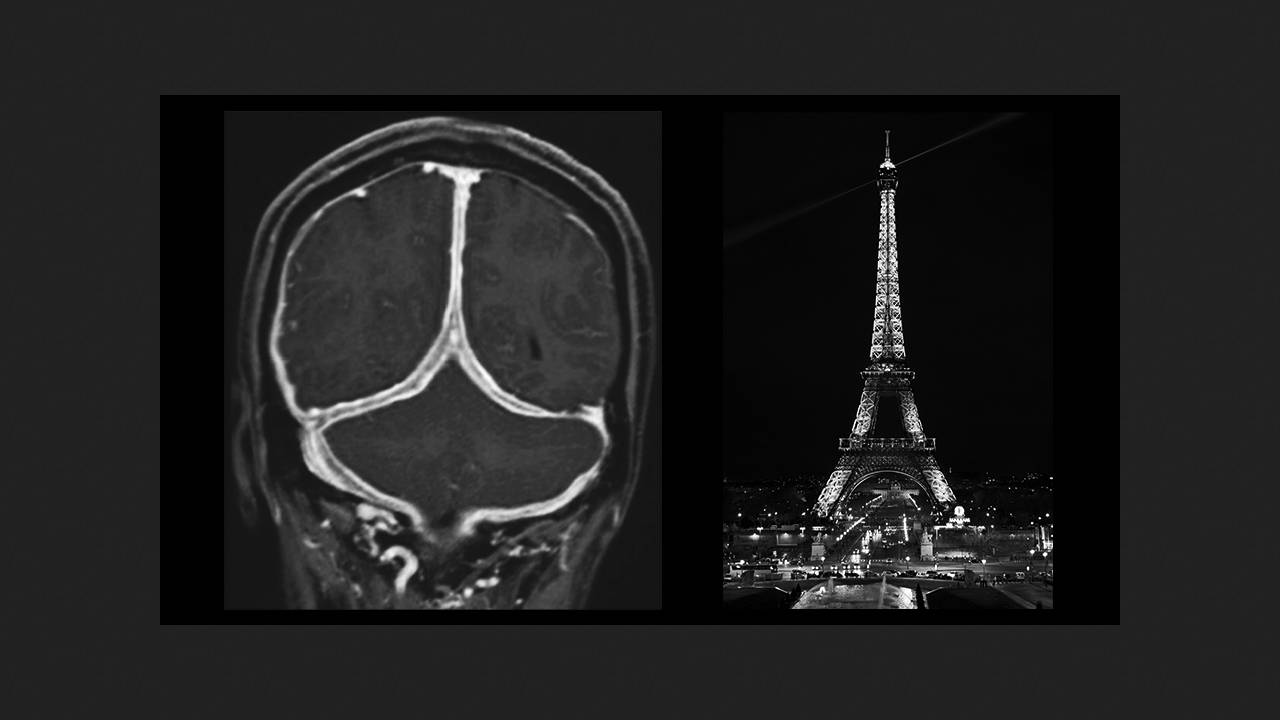
A 50-year-old man sought medical attention in China with complaints of headaches and nausea that had been progressing for a year. Examination revealed neck muscle rigidity and dysmetria (failure to reach the finger-to-nose test) in both hands. A lumbar puncture revealed elevated cerebrospinal fluid pressure (CSF) to 310 mmH2O (normal range: 70–200 mmH2O), as well as elevated protein levels and immunoglobulin levels. A contrast-enhanced MRI revealed a thickened dura mater with central hypointensity and peripheral enhancement in the posterior falx cerebri and tentorium cerebelli—a pattern known as the Eiffel Tower sign. Kundian Guo and Zhen Hong of Sichuan University Hospital shared their case in The New England Journal of Medicine.
This sign is considered pathognomonic for acute inflammation in chronic pachymeningitis, which can be inflammatory, autoimmune, neoplastic, or vascular in nature. A dura mater biopsy revealed lymphoplasmacytic infiltration with IgG4-positive plasma cells, and elevated serum antibody levels. A full-body MRI revealed no involvement of other organs. Based on these findings, the patient was diagnosed with IgG4-associated hypertrophic pachymeningitis. He received pulse methylprednisolone for five days, followed by a gradual tapering of the dose to oral glucocorticoids. Two months later, the MRI showed improvement, and six months later, the headaches resolved with a maintenance dose of medication.