German, Spanish, Czech, and Swiss researchers reported the completion of a phase II clinical trial of monoclonal antibodies for the rehabilitation of patients with cervical spinal cord injuries. Overall, the drug did not demonstrate significant efficacy, but participants with partial motor loss demonstrated potential benefit, which merits further study with dose adjustments. The study was published in The Lancet Neurology.
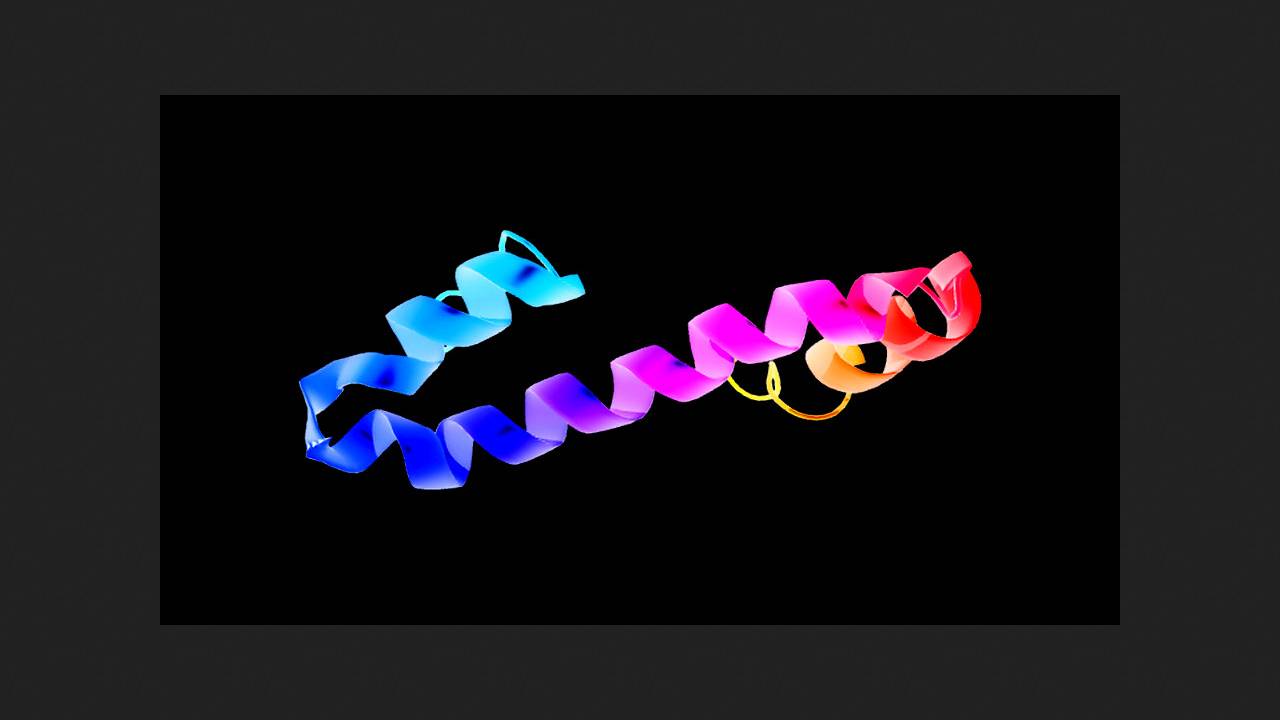
After spinal cord injury, the nerve fibers within it fail to regenerate, leading to persistent movement and sensory impairments below the injury site. Cervical spine injuries have the worst consequences, impairing the function of both the lower and upper extremities. The failure of nerve fiber regeneration after injury is largely due to inhibition by endogenous molecules. One of the most important such inhibitors is Nogo-A, an isoform of the membrane protein reticulon-4 (Nogo), widely present in the myelin sheaths of nerve fibers.
The experimental anti-Nogo-A monoclonal antibody NG101 (ATI355) demonstrated high neutralizing activity in both in vitro and in vivo experiments, promoting partial motor recovery after spinal cord injury in rodents and non-human primates. Phase I clinical trials confirmed its satisfactory tolerability and safety profile.
Norbert Weidner of Heidelberg University Hospital and colleagues conducted a double-blind, randomized, placebo-controlled phase 2b trial at 13 clinics in Germany, Spain, the Czech Republic, and Switzerland. They enrolled 126 patients aged 18–70 years with acute (4–28 days after injury) cervical spine injury with complete or partial loss of motor function. The extent of injury was determined using MRI and cerebrospinal fluid analysis for neurofilament light chain (NfL).
When selecting participants, the authors used an unbiased recursive partial analysis to exclude those whose peak motor function recovery was expected within the next six months (as the drug was highly unlikely to provide any benefit to them). Seventy-eight patients, starting 28 days after injury, received six intrathecal injections of 45 milligrams of NG101 at five-day intervals in addition to standard treatment; the remaining 48 received placebo according to the same regimen. The primary endpoint was upper limb motor function, as measured by the UEMS, six months after injury.
On average, no statistically significant differences were observed between groups for the primary endpoint, nor for changes in MRI imaging or NfL concentrations. The incidence of adverse events (most commonly infections), including severe ones, was also comparable. Furthermore, a subgroup analysis showed that in cohorts that included only patients with partial loss of motor function, the treatment effect was significant: the improvement in the UEMS was 4.40 points (95% confidence interval 1.32–7.47), and in the SCIM self-care scale, it was 4.16 points (95% confidence interval 1.95–6.36).
Among these participants, 18 percent of those receiving active treatment were in the least independent category on the SCIM at day 168, compared to 32 percent receiving placebo, and 45 percent were in the most independent category, compared to 28 percent. Analysis of NG101's pharmacokinetic properties showed that its half-life in cerebrospinal fluid is relatively short, approximately 10–11 hours, preventing steady-state concentrations from being achieved with the regimen used.
Taking into account the data obtained, the authors of the study concluded that it makes sense to continue testing the drug in patients with partial loss of motor functions after adjusting the dosage regimen taking into account the identified pharmacokinetics.
Previously, American and Swiss scientists successfully targeted the regeneration of damaged axons and restored walking ability in mice after a complete transection of the spinal cord in the lower thoracic region. The mice also showed improvement with the administration of polylactide-co-glycolide nanoparticles. Other experimental approaches include the use of stem cells and neural interfaces.